EU-wide Task Force publishes work programme 2019/20 and prepares multi-stakeholder workshop
National Competent Authorities (NCAs) launched a fast-track approach for the authorization of multinational clinical trials in the EU/EEA
Yesterday, a large number of National Competent Authorities (NCAs) and Ethics Committees committed to test a coordinated fast-track approach for evaluating multinational clinical trials.
This approach, known as FAST-EU (Facilitating and Accelerating Strategic Trials), is part of the overall EU drive to strengthen clinical research in Europe. It is coordinated with the European Commission’s upcoming legislative initiative to streamline procedures for multi-national clinical trials in the EU.
The FAST-EU approach foresees clear and ambitious timelines and coordination mechanisms. The goal is to provide trial sponsors with greater predictability in evaluation and authorisation timelines, strengthen sponsors’ confidence in the European regulatory system and facilitate the attraction of research investment while maintaining scientific, safety and ethical standards.
The initiative is expected to start in January 2026, and will be part of the wider efforts to enhance collaboration and reliance between national medicines authorities, with the support of the EU.
In this way, FAST-EU aims to demonstrate the EU’s capacity for coordination and rapid response, reinforce Europe’s global competitiveness in biomedical research, and ensure that European patients benefit sooner from scientific advancements and therapeutic innovation. It also sends a clear signal of commitment to innovation and cooperation within and across member states. In contrast to other regions in the world Ethics Committees´ opinions of all participating member states are already built into this ambitious process.
Multinational clinical trials account for a significant share of authorised studies in Europe. These studies are important, as they enable a sufficient number of patients to be recruited across different countries to obtain robust results and accelerate the development of innovative treatments. Facilitating clinical trials in Europe also guarantees the inclusion and representation of European patients in the development of these therapies.
Further details will be communicated through HMA channels in due time.
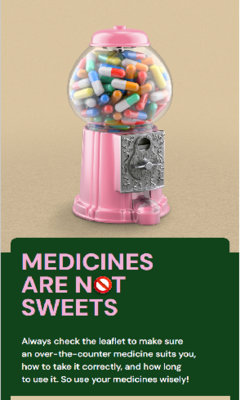
Medicines are not sweets: European campaign promoting responsible use of over-the-counter medicines
Read the leaflet, follow the instructions, and use (over-the-counter) medicines wisely. That is the joint message from European medicines authorities involved in the campaign. The campaign aims to raise awareness among European citizens about the importance of proper use of over-the-counter (OTC) medicines.
The campaign targets everyone who occasionally uses OTC medicines such as painkillers, nasal sprays, antacids, or cough syrup.
What are over-the-counter medicines?
Over-the-counter medicines can be purchased without a prescription from a pharmacy, drugstore or supermarket. These medicines are intended for mild health complaints such as pain, fever, or a cold. However, no medicine is without risk. Incorrect use can lead to unpleasant side effects or even addiction. That is why it is important—just as with any medicine—to read the patient information leaflet carefully and follow the instructions.
European cooperation
Since the use of OTC medicines crosses borders, European countries have joined forces in this campaign. It underscores the essential steps for a safer use of these medicines: reading the leaflet, adhering to the recommended maximum duration of use, and consulting a doctor if symptoms persist.
“Medicines are not sweets” is the first joint campaign launched by the Heads of Medicines Agencies (HMA).
About HMA
The Heads of Medicines Agencies (HMA) is a network of national authorities in Europe who are involved in the registration of medicines. HMA works closely with the European Medicines Agency (EMA) and the European Commission to ensure the safety, quality, and effectiveness of medicines.
Warning about sharp rise in illegal medicines sold in the EU
Illegal medicines marketed as GLP-1 receptor agonist for weight loss and diabetes pose serious risk to health.
EMA and the Heads of Medicines Agencies (HMA) are warning the public about the growing threat of illegal medicines being advertised and sold online across the European Union.
In recent months there has been a sharp rise in the number of illegal medicines marketed as GLP-1 receptor agonist such as semaglutide, liraglutide and tirzepatide for weight loss and diabetes. These products, often sold via fraudulent websites and promoted on social media, are not authorised and do not meet necessary standards of quality, safety and efficacy.
Such illegal products pose a serious risk to public health. They may not contain the claimed active substance at all and may contain harmful levels of other substances.
People who use these products are therefore at a very high risk of treatment failure, unexpected and serious health problems and dangerous interactions with other medicines.
Authorities have identified hundreds of fake Facebook profiles, advertisements and e-commerce listings, many of which are hosted outside the EU. Some fraudulent websites and social media advertisements misuse official logos and use false endorsements to mislead consumers. Illegal suppliers are being actively monitored by national authorities. Enforcement actions include ordering product withdrawals, blocking websites and cross-border collaboration with enforcement officers and other international partners.
GLP-1 receptor agonists are prescription medicines for serious health conditions such as diabetes and obesity. Online sales of prescription only medicines is not allowed in all Member States, and buyers must comply with the legislation applicable on their country of residence. They should be taken under the supervision of a healthcare professional. Patients who think they might benefit from treatment with GLP-1 receptor agonists should discuss with a doctor and should not buy them without a prescription or from sources other than legitimate retailers.
Unregulated advanced therapy medicinal products pose serious risks to health
Unregulated advanced therapy medicinal products pose serious risks to health
Authorities warn about unregulated products in the EU, including dendritic cell cancer therapies
EMA and the Heads of Medicines Agencies (HMA) are warning the public about the dangers of unregulated advanced therapy medicinal products (ATMPs) offered to patients in the European Union.
ATMPs are medicinal products that are based on genes, tissues or cells. When these medicines are regulated (i.e. authorised via EMA or approved by a national authority), they can offer important benefits for patients. The European Union has established guidelines to ensure that ATMPs meet stringent safety and efficacy standards.
However, a number of individuals, companies and clinics have been marketing unregulated ATMPs directly to patients, often when there is little or no evidence that the products work or are safe. Some of the unregulated products in the EU are sold as dendritic cell therapies, which use a type of immune cell (dendritic cell) to attack cancer cells.
Authorities are warning the public that unregulated products could put patients at risk, causing serious side effects while not providing benefits to patients. Additionally, unregulated ATMPs present significant quality-related risks due to the lack of strict oversight and regulatory compliance in the manufacturing process, which can lead to contamination, inconsistent product composition, and improper storage. Patients may also face substantial financial costs and emotional distress from ineffective or harmful treatments.
It is important that patients are only offered ATMPs, including dendritic cell therapies, that have been authorised or approved by a regulator.
HMA/EMA guidance document on the identification of personal data and commercially confidential information within the structure of the marketing authorisation application (MAA) dossier
In 2023, the Heads of Medicines Agencies (HMA) and the European Medicines Agency (EMA) agreed to update the guidance originally adopted in 2012 regarding the classification of personal data (PD) and commercially confidential information (CCI) in the Marketing Authorisation Application (MAA) dossiers for medicinal products intended for human use.
This revision was prompted by insights gained over the past decade through the application of the principles set out in the 2012 guidance document. It became clear that updates were needed to ensure the guidance and its annex remain aligned with current practices and regulatory expectations.
The primary objective of this update is to continue fostering a common and consistent approach across the European Economic Area (EEA). The revised guidance provides clear instructions for identifying PD that must be protected, as well as considerations regarding CCI within MAA dossiers, in line with transparency obligations.
This guidance document applies to information and documents related to medicinal products for human use, specifically those for which the regulatory procedures have been completed under national, mutual recognition, decentralised, or centralised procedures.
Access the updated guidance document here.
Read the announcement on the EMA website.
Letter from the HMA Core Group for Medical Devices to the European Commission
Correspondence emphasizes the readiness of the national authorities responsible for medical devices to collaborate with the European Commission and relevant partners to address the challenges identified within the current regulatory framework. It highlights the urgent need for thoughtful and deliberate action, particularly in light of recent discussions in the European Parliament regarding the revision of medical device legislation. The letter articulates concerns about the potential for hastily expedited amendments that may further complicate the regulatory landscape and may have unintended impact on public health. It underscores the necessity for comprehensive analysis and impact assessments, including the Commission's ongoing targeted evaluation, to ensure that any legislative changes are aligned with core objectives and do not inadvertently create further challenges.
The Competent authorities remain committed to identifying actions that can be taken in the short and medium term to address, at least in part, the issues and concerns raised by stakeholders. They will continue to work intensively with relevant teams in progressing these in the short term and in advance of completion of the targeted evaluation.
The full text is available on the following LINK.
European medicines agencies network strategy to 2028 – launch of public consultation
EMA and the Heads of Medicines Agencies (HMA) have published their draft joint EU network strategy to 2028 for an eight-week public consultation.
This is a review and update to the original five-year strategy, which was developed to cover the period 2021 to 2025 (EMANS 2025). Since then, several changes to the regulatory and technological landscape have occurred, some more rapidly than anticipated. For example, the European Union has enacted new legislation to handle public health emergencies and established the Directorate-General for Health Emergency Preparedness and Response (DG HERA) to improve the EU’s crises preparedness. Technological advances, particularly in artificial intelligence, have presented opportunities to transform the way medicines are developed and regulated across the network. Furthermore, the EU has made steps to revise its pharmaceutical legislation in the largest reform of the EU medicines regulation in decades. These changes made it necessary to update the EMANS 2025 and to seize the opportunities that they present.
“The overarching theme of our updated strategy to 2028 is that of change – rapid, somewhat unpredictable but nonetheless full of promise,” said Emer Cooke, EMA’s Executive Director. “It will guide the network as it seizes opportunities and meets the challenges of the near future, including preparing for and responding to public health emergencies and threats such as antimicrobial resistance. Now is the time to share your views and help shape the direction of the network for the next few years.”
The strategic focus areas of the strategy to 2028, are as follows:
Accessibility – to facilitate pathways for access to medicines through healthcare systems in the EU.
Leveraging data, digitalisation and artificial intelligence – to improve decision-making, optimise processes and increase efficiency.
Regulatory science, innovation and competitiveness – to create a regulatory and research environment that improves innovation and competitiveness of the EU’s healthcare sector.
Antimicrobial resistance and other health threats – to prepare the EU for potential threats including antimicrobial resistance.
Availability and supply - to strengthen the availability of medicines to protect public and animal health.
Sustainability of the network – to ensure that the network has available resources to support its scientific and regulatory decision making.
“The six focus areas have been carefully chosen to support the network’s core work of evaluating medicines as we take strides to promote the development of medicines and ensure that they reach those who need them,” added Maria Lamas, Chair of the HMA Management Group.
Input on the draft strategy is welcome from all stakeholders until 30 November 2024 via an online questionnaire.
EMA and the HMA will evaluate progress in each focus area by assessing how they achieve the goals set out in the strategy and will adapt their approaches as necessary to advances in science and technology, as well as to new opportunities that arise.
The updated strategy replaces the current network strategy to 2025 and incorporates the strategic aspects of EMA’s Regulatory Science Strategy. It takes into account progress made so far with the EMANS 2025 (as outlined in the mid-term report) and has been developed with input from experts from across the EU medicines regulatory network. More information on the drafting process and considerations driving the EMANS 2028 is included in a reflection paper, which is also published today to support the consultation on the draft strategy.
The draft strategy was endorsed by the HMA in September 2024 and by EMA’s Management Board at its 3 October 2024 meeting.
Following the eight-week public consultation, EMA and the HMA will finalise the strategy and it will be implemented via EMA’s and HMA’s respective multi-annual workplans.
EMA and HMA expect to adopt the final strategy by March 2025.
Notes
This press release, together with all related documents, is available on the two agencies’ websites.
Related documents
Seizing opportunities in a changing medicines landscape: The European medicines agencies network strategy 2028 (draft) - View
European Union Medicines Agencies Network Strategy to 2025 - Protecting public health at a time of rapid change - View
Towards the European medicines agencies network strategy 2028: Reflection paper - View
Contact our press officers
Heads of Medicines Agencies Permanent Secretariat
E-mail: ps@hma.eu
EMA press office
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Medical Devices and In Vitro Diagnostics Regulations: publication of a consensus statement from the EU Competent Authorities to the EU Commission
National Competent Authorities have endorsed a consensus statement and shared it with the European Commission on the status of the EU regulatory framework for medical devices. This consensus statement outlines common priorities for future actions to implement and current challenges to overcome.
On July 10th 2024, Competent Authorities as well as representatives from the EU Commission gathered in a workshop in France to discuss the implementation of the European Regulations for medical devices (2017/745) and in-vitro diagnostics devices (2017/746).
The goal was to do a state-of-play on the Regulations with the ambition to contribute to the targeted evaluation conducted by the EU Commission. It was organized at the instigation of the HMA Core Group and supported by the EU Commission.
This workshop was centred around 4 thematic pillars: Access & availability, Safety, Innovation as well as Governance & coordination that led to the drafting of a consensus statement.
With this statement, National Competent Authorities acknowledge the difficulties in the application of the regulations but wish to reiterate their confidence in the regulatory framework set out for medical devices and IVDs, underline the importance of the Regulations in the protection of public health but also outline the way forward to make the regulatory system work effectively.
National Competent Authorities remain committed to support the European Commission and work, as necessary, with key stakeholders for the effective application of the Regulations.
- List of Heads with the Consensus statement (updated version 9/2024)
European medicines network designated as WHO listed authority
The European Medicines Regulatory Network (EMRN) has been designated as WHO Listed Authority (WLA) by the World Health Organization (WHO).
This means that the network, composed of the European Commission, EMA and the 30 national authorities of the European Economic Area Member States, are recognised as meeting international regulatory standards, guidelines and practices.
European medicines network designated as WHO listed authority
EU medicines agencies reflect on lessons learned from COVID-19
The European Medicines Regulatory Network (EMRN) has been at the forefront of the fight against COVID-19 with its crucial role in the evaluation and monitoring of medicines, including vaccines. A joint report issued by EMA and the Heads of Medicines Agencies (HMA) reviews the Network’s response and highlights the main learnings for any future health crises.
This review highlights some of the unprecedented challenges related to COVID-19 that had to be addressed, the activities and areas that enabled the effective response to the COVID-19 emergency and provides recommendations on which improvements are needed.
Accelerated procedures for the evaluation of COVID-19 vaccines and therapeutics, as well as scientific recommendations on the use of certain medicines enabled the public health response through safe and effective prevention and treatment options.
The Network pooled its resources to address the increased workload and new tasks like managing medicine shortages, generating evidence on COVID-19 medicines in the real-world setting and regularly providing reliable and science-based information to the public.
Additionally, the EU safety monitoring and risk management system was strengthened to collect and monitor the high volume of data from the mass vaccination campaigns. This allowed the Network to promptly identify, assess and manage safety issues.
Collaboration between EU and international partners was also crucial to ensure that regulators around the world adopted a coordinated approach to COVID-19 treatments and vaccines.
Throughout the COVID-19 crisis, the EMRN also ensured that medicines for other diseases affecting Europeans continued to be evaluated and supervised without delays.
The report suggests that more can be done in terms of the ability to set up large clinical studies in a rapid manner. In terms of real-world data, there is a need to gather multiple data sources that can generate useful evidence for regulatory assessments.
The report also acknowledges the need to have a larger pool of experts that can be involved to carry out scientific assessments (such as accelerated reviews for promising medicines) when crisis situations arise.
The report has been adopted by EMA’s Management Board. Several recommendations have already been implemented as part of EMA’s extended mandate, with the Agency assuming an enhanced role on preparedness to be more proactive on public health threats. HMA and EMA also continue working closely on areas such as resourcing, process improvements and communication. In addition, the ongoing review of the EU pharmaceutical legislation will also provide a vehicle to bring about other changes to the EU regulatory toolbox. The recommendations will also be considered in future updates of the European Medicines Agencies Network strategy.
COVID-19 lessons learned: Joint report on the response to the public health emergency | pdf
Notes
1. This press release, together with all related documents, is available on the two agencies’ websites.
Contact
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
EMA press office
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Reflection paper on the use of artificial intelligence in the lifecycle of medicines
EMA has published a draft reflection paper outlining the current thinking on the use of artificial intelligence (AI) to support the safe and effective development, regulation and use of human and veterinary medicines. This paper, which is now open for public consultation, reflects on principles relevant to the application of AI and machine learning (ML) at any step of a medicines’ lifecycle, from drug discovery to the post-authorisation setting.
The reflection paper is part of the joint HMA-EMA Big Data Steering Group (BDSG) initiatives to develop the European Medicines Regulatory Network’s capability in data-driven regulation. It has been developed in liaison between the BDSG, EMA’s Committee for Medicinal Products for Human Use (CHMP) and its Committee for Veterinary Medicinal Products (CVMP).
"The use of artificial intelligence is rapidly developing in society and as regulators we see more and more applications in the field of medicines. AI brings exciting opportunities to generate new insights and improve processes. To embrace them fully, we will need to be prepared for the regulatory challenges presented by this quickly evolving ecosystem" said Jesper Kjær, Director of the Data Analytics Centre at the Danish Medicines Agency and co-chair of the BDSG. "With this paper, we are opening a dialogue with developers, academics, and other regulators, to discuss ways forward, ensuring that the full potential of these innovations can be realised for the benefit of patients’ and animal health" said Peter Arlett, EMA’s Head of Data Analytics and Methods, co-chair of the BDSG.
AI and ML tools have the potential to effectively support the acquisition, transformation, analysis, and interpretation of data across the medicinal product lifecycle. Their application can include, for example, AI/ML modelling approaches to replace, reduce, and refine the use of animal models during the preclinical development. In clinical trials, AI/ML systems may support the selection of patients based on certain disease characteristics or other clinical parameters; AI/ML tools can also support data recording and analyses which will in turn be submitted to regulators in marketing-authorisation procedures.
At the marketing-authorisation stage, AI applications include tools to draft, compile, translate, or review data to be included in the product information of a medicine. In the post-authorisation phase, such tools can effectively support, for example, pharmacovigilance activities including adverse event report management and signal detection.
This range of applications brings with it challenges such as the understanding of the algorithms, notably their design and possible biases, as well as the risks of technical failures and the wider impact these would have on AI uptake in medicine development and health.
The reflection paper highlights that a human-centric approach should guide all development and deployment of AI and ML. The use of AI in the medicinal product lifecycle should always occur in compliance with the existing legal requirements, consider ethics and ensure due respect of fundamental rights.
If an AI/ML system is used in the context of medicines’ development, evaluation, or monitoring, and is expected to impact on the benefit-risk balance of a medicine, EMA advises developers to seek early regulatory support, e.g. through qualification of innovative development methods (for human medicines) or scientific advice.
All interested stakeholders are invited to comment on the draft reflection paper and to identify opportunities and risks of AI in the field of medicines. The public consultation is open until 31 December 2023 and the topic will be further discussed during a joint HMA/EMA workshop scheduled for 20-21 November 2023. The feedback from stakeholders will be analysed and considered for the finalisation of the reflection paper and future development of guidance as relevant.
Reflection paper on the use of Artificial Intelligence (AI) in the medicinal product lifecycle | pdf
Contact
Heads of Medicines Agencies Permanent Secretariat
E-mail: ps@hma.eu
European Medicines Agency
Media enquiries
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
All other enquiries
Please submit your request via the online form
Follow us on Twitter @EMA_News
Shaping a European innovation ecosystem: EU-Innovation Network multi-stakeholder meeting
The EU Innovation Network (EU-IN) and the Spanish Agency of Medicines and Medical Devices (AEMPS) are organising a multi-stakeholders meeting under the Spanish 2023 EU-Presidency to promote research and development of innovative medicines and related technologies & methodologies in the European Union.
The meeting will take place on the 26th September 2023, under the title: Shaping a European innovation ecosystem: EU-Innovation Network multi-stakeholder meeting. This full day event will be held in a hybrid format, face to face in Madrid, as well as virtually.
The main objectives of the meeting are:
- To inform stakeholders on EU-IN activities and available EU regulatory support to developers and to gather feedback on how to further optimise these support tools;
- To exchange knowledge, experience and good practices among stakeholders involved in medicines research and development and explore opportunities for collaboration;
- To collect inputs from multiple stakeholders, in particular from academic innovators, to identify gaps in regulatory science and discuss options to address them.
The feedback gathered during this meeting will inform recommendations and follow-up actions with the aim to further catalyse innovative medicines development in the European Union.
Registration will be available shortly.
Draft agenda | pdf
Further information on the meeting can be found under the following links:
- AEMPS website (Spanish, English)
- EMA's website
Use of real-world evidence in regulatory decision making – EMA publishes review of its studies
Real-world evidence (RWE) from studies led by regulators can complement evidence from other sources including clinical trials. RWE can support both pre-authorisation and post-approval assessments of EMA’s scientific committees, working parties and national competent authorities. However, more effort is needed to better anticipate the need for such studies and to speed up their initiation to ensure that regulators have access to RWE in a timely manner.
These are some of the findings of a report published today on the experience EMA has gained in conducting studies with real-world data (RWD) in the past year and a half. The report is part of the Agency’s efforts, alongside the European Medicines Regulatory Network (EMRN), to enable use of RWD in regulatory decision making.
In pharmacovigilance, it has become mainstay to use routinely collected data about a patient’s health status or the delivery of healthcare from a variety of sources other than traditional clinical trials to support decision making. However, the use of RWE is less established in earlier stages of medicines development.
Overseen by the EMA-HMA Big Data Steering Group, EMA and EMRN are working towards setting up a sustainable framework that enables the use and establishes the value of RWE in decision making across the entire product lifecycle.
Since the completion of an earlier pilot with the Pharmacovigilance Risk Assessment Committee (PRAC) in 2021, EMA has engaged in various pilots with its other scientific committees and working parties. The pilots aim to explore the need for and usefulness of RWE generated by EMA to support regulatory decisions. While the pilots continue, the report takes stock of the experience gained so far with regulator-led RWD studies. It focuses on studies conducted in addition to those performed in response to the COVID-19 public health emergency and the Pharmacovigilance impact strategy.
The report covers the period from September 2021 until the first anniversary of the Data Analysis and Real-World Interrogation Network DARWIN EU® on 7 February 2023. During this period, 61 RWD research opportunities were identified, 30 studies initiated and 27 completed.
The review considers studies conducted via EMA’s three pathways for RWE generation:
- 25 studies were initiated by EMA through a team of pharmacoepidemiologists and data scientists using six databases containing mainly primary care medical records from European countries;
- Four studies were initiated via DARWIN EU®;
- One study was commissioned to one of the eight research organisations and consortia with which EMA has framework contracts in place to commission research.
While most research topics were related to scientific assessments of the PRAC, research opportunities were identified across the spectrum of EU decision-makers, including one pilot study in preparation via DARWIN EU® to support health technology assessment bodies and payers organisations.
Studies performed included safety, drug utilisation and disease epidemiology studies, as well as studies to inform the design and feasibility of clinical trials and clinical management. Most studies conducted focused on conditions diagnosed or medicines used in the primary care setting. For about a third of the research topics, a study was not considered feasible, for example because the medicines or the outcomes of interest were not adequately captured in the available databases, or due to procedural time constraints.
The report provides a set of recommendations to address identified opportunities and challenges. These include the need for wider access to additional and complementary data sources, strategies to further accelerate RWE generation as well as earlier identification of research needs, tools to further build capability and capacity for RWE generation and close collaboration with decision-makers and other stakeholders.
Further work is needed to fulfil the European Union’s vision to enable the use of RWE and establish its value across regulatory use cases by 2025. The learnings and recommendations arising from the review will feed into the work of the Big Data Steering Group and further inform the establishment of DARWIN EU®.
Notes
The report will be discussed during the Multi-stakeholder workshop on Real World Data (RWD) quality and Real World Evidence (RWE) use on 26-27 June. Interested stakeholders are invited to follow the live broadcast of the workshop.
Real-world evidence framework to support EU regulatory decision-making: Report on the experience gained with regulator-led studies from September 2021 to February 2023 | pdf
Contact
Heads of Medicines Agencies Permanent Secretariat
E-mail: ps@hma.eu
European Medicines Agency
Media enquiries
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
All other enquiries
Please submit your request via the online form
Follow us on Twitter @EMA_News
ACT EU: creating a better environment for clinical trials through collaboration
The Accelerating Clinical Trials in the EU (ACT EU) initiative is today organising the kick-off workshop for a new multi-stakeholder platform to improve clinical trials in the European Union (EU). ACT EU is a collaboration between EMA, the Heads of Medicines Agencies (HMA) and the European Commission (EC) that seeks to transform how clinical trials are initiated, designed, and run. The multi-stakeholder platform is a key deliverable of the initiative.
ACT EU aims to place stakeholders at the centre of its activities by giving them the opportunity to steer the direction of the programme. Today’s workshop will discuss best approaches to support the implementation of the clinical trial regulation including the role of ethics committees, support to non-commercial sponsors to increase the conduct of multinational clinical trials and how to optimise the coordination of scientific advice to support evidence generation.
Peter Arlett, Head of Data Analytics and Methods Task Force at EMA, said: “The multi-stakeholder platform will build consensus and enable new approaches to clinical studies positioning the EU as a preferred location for innovative clinical research.”
Björn Eriksson, HMA’s lead on clinical trials: “A successful clinical trials environment in all Member States will support bigger, better and faster clinical trials for better medicines for patients and drive innovation and investment.”
Sylvain Giraud, Head of Unit at the EC’s Directorate-General for Health and Food Safety: “The multi-stakeholder platform provides the opportunity for a dialogue at EU level to exchange on the implementation of the Clinical Trials Regulation and ensure compliance with its rules and modalities.”
A series of public events bringing together clinical trials stakeholders will be organised during 2023 and 2024 to discuss and agree the model for the establishment of the platform.
Background
ACT EU was launched in January 2022 and aims to further develop the EU as a focal point for clinical research, to promote the development of high-quality, safe and effective medicines, and to better integrate clinical research in the European health system. ACT EU features ten priority action areas that are the basis for the ACT EU 2022-2026 workplan.
Notes
- This press release, together with all related documents, is available on the Agency's website.
- Any queries related to the multi-stakeholder platform should be directed to ACTEU@ema.europa.eu
- More information on the work of the European Medicines Agency can be found on its website: www.ema.europa.eu
Contact
Media enquiries
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
All other enquiries
please submit your request via the online form
Follow us on Twitter @EMA_News
Enabling oncology scientists' participation in medicine regulation (pilot project) (new)
EMA and the Heads of Medicines Agencies (HMA) are running a pilot project to enable clinical-oncology scientists to participate in medicine regulation. The pilot aims to achieve this by providing them with an understanding of basic principles relevant to their field.
The pilot focuses on scientific advice and marketing authorisation assessments for human medicines.
Prospective candidates must have experience in clinical oncology or haemato-oncology.
They do not need to have any prior understanding of regulatory requirements in medicine evaluation.
The pilot consists of live and recorded webinars covering the following areas:
- Basic principles of the regulation of human medicines in the EU
- Basic regulatory aspects relevant to oncology
Prospective candidates can apply by completing a brief registration form.
Participation is free of charge.
EMA and HMA launched the pilot in May 2023. It will be rolled out over 12 months.
It aims to increase collaboration between regulatory authorities and stakeholders in healthcare and academia, in line with the recommendations of the STARS common strategy.
EMA and European medicines regulatory network lift COVID-19 business continuity status
EMA and the European medicines regulatory network are lifting their respective COVID-19 business continuity measures after successfully handling the unprecedented operational challenges posed by the pandemic. This was foreseen in EMA’s workplan for 2023-2025.
EMA's business continuity plan was introduced in 2020 to ring-fence resources to deal with COVID-19 while safeguarding the continuity of EMA's core activities related to the evaluation and supervision of medicines during the pandemic. It was originally put in place to prepare for the relocation of EMA from the United Kingdom to the Netherlands and operational changes linked to Brexit.
The business continuity plan for the European medicines regulatory network is also being lifted. This plan set out the principles to ensure that EMA, the European Union (EU) Member States and the European Commission could continue to operate their core regulatory activities while prioritising the assessment of COVID-19 treatments and vaccines to protect public and animal health in the EU during the pandemic.
EMA is gradually reinitiating activities that were suspended or reduced, including the planned restart of clinical data publication for all new active substances later this year. EMA’s workplan for 2023 to 2025 outlines the focus of the Agency’s work over the next two years.
Since the initiation of its business continuity plan in 2020, EMA’s mandate has been extended to include the work of its Emergency Task Force (ETF), engagement with national competent authorities and stakeholders in tackling medicines shortages, as well as new tasks in the field of medical devices. This is a direct recognition of the activities undertaken by EMA on its own initiative during the pandemic to address pressing public health needs. The resource needs for these additional activities are covered as part of the extended mandate and lifting of the business continuity plan will not affect these areas.
While the temporary measures that were introduced to cope with the peak impact of the COVID-19 pandemic are no longer required, resourcing within the entire European medicines regulatory network remains a challenge. EMA and the Heads of Medicines Agencies will continue to work closely to identify and implement sustainable solutions. Experiences gathered during application of the EMA and network business continuity plans, as well as lessons learnt during the pandemic, will inform this work.
The lifting of the COVID-19 business continuity measures is timely in view of World Health Organization (WHO)'s recent announcement on the end of the Public Health Emergency of International Concern (PHEIC) status of COVID-19.
Contact
Heads of Medicines Agencies Permanent Secretariat
E-mail: ps@hma.eu
European Medicines Agency
Media enquiries
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
All other enquiries
Please submit your request via the online form
Follow us on Twitter @EMA_News
HMA Core Group for medical devices Statement on effective application of the EU regulatory system for medical devices
Statement on effective application of the EU regulatory system for medical devices
Launch of phase 2 of the Simultaneous National Scientific Advice pilot
The EU Innovation Network (EU IN) has launched phase 2 of the simultaneous national scientific advice (SNSA) pilot. SNSA is intended to be used in situations where an applicant wishes to obtain national scientific advice from more than one NCA at the same time. The format is intended to enhance the quality and consistency of such advice. Following endorsement by the Heads of Medicine Agencies (HMA), phase 2 of the SNSA pilot will run for a two-year period until the end of 2024. Phase 2 incorporates an optimised procedure intended to maximise the benefits for both applicants and competent authorities.
In conjunction with the ACT-EU initiative, this phase of the SNSA pilot will have a specific focus on scientific advice to facilitate clinical trials (CT) within Europe. It will facilitate sponsors / developers to obtain clinical trial-related national scientific advice from National Competent Authorities (NCA) in Member States (MS) where they intend to perform clinical trials. The experience gained during the SNSA pilot will be used to further develop the process and the provision of clinical trial-related advice as part of ACT EU Priority Action 7 (ACT EU PA7). The following are examples of scenarios where developers may choose to seek SNSA:
- In preparation for clinical trials (CT) applications to be performed in more than one MS. Where during the SNSA the involved NCAs agree that the questions raised would benefit from discussions at the Clinical Trial Coordination Group (CTCG) level, it is also possible to obtain CTCG-coordinated clinical trial expert feedback as part of the SNSA procedure.
- Prior to applying for funding grants to support non-commercial clinical trials (academic researchers).
- To inform the early-stage development of innovative products for which clinical trials are planned, e.g. phase I / II clinical trials, especially where there is limited existing regulatory guidance. EMA scientific advice should continue to be used for scientific advice related to the suitability of the proposed clinical development to support a centralized marketing authorisation application.
- Prior to clinical trials intended to facilitate repurposing of authorised medicinal products e.g. to support new innovative therapeutic indications
Phase 2 of the SNSA pilot builds on the success of the first phase of the pilot, it optimizes the procedure, while maintaining the key principles associated with SNSA. The pilot is open to applicants from different backgrounds including large pharmaceutical companies, while strongly encouraging SMEs and especially inviting academic research centres and hospitals to join. Within each SNSA procedure, each participating NCA will prepare and discuss their positions on the questions raised by the applicant with a view to maximising alignment prior to a joint advice meeting with the applicant. Where divergent positions remain, these will be explained to the applicant in the joint advice meeting and subsequently be summarised in consolidated meeting minutes with a view to facilitating further consideration and appropriate follow-up upon agreement of the applicant.
The optimized pilot SNSA process will continue to complement and provide a bridge between purely national scientific advice and centralised European scientific advice procedures from EMA as well as supporting the aims of the ACT-EU initiative and the CTCG.
How to apply for SNSA:
Guidance on how to prepare and submit a formal SNSA request and relevant templates are listed below:
- Guidance to applicants
- Guidance on SNSA briefing book format and content
- List of participating NCA’s and contact info
- Application form
For any further information, please contact SNSA@pei.de.
Additional information can be found in the EU-Innovation Network (EU-IN) section of the HMA website, as well as on EMA website.
Big data use for public health: publication of Big Data Steering Group workplan 2022-25
The Big Data Steering Group set up by the European Medicines Agency (EMA) and the Heads of Medicines Agencies (HMA) has published its third workplan that sets key actions to be delivered between 2022–25.
The new workplan will allow to further enhance the efficient integration of data analysis into the evaluation of medicinal products by regulators. Using novel technologies and the evidence generated from big data will benefit public health by accelerating medicine development, improving treatment outcomes and facilitating earlier patient access to new treatments.
The former Big Data Task Force carried out a thorough assessment of the challenges and opportunities posed by big data in medicines regulation, which culminated in 2020 in the publication of priority recommendations for regulators on the best approaches to use and generate data. The joint HMA-EMA Big Data Workplan 2022–2025 follows the key recommendations and includes mainly activities related to medicines for human use. However, the scope of some activities covers veterinary aspects, and a separate section in the workplan is fully dedicated to veterinary medicines.
The workplan lays out deliverables and timelines including for the following areas:
- The Data Analysis and Real World Interrogation Network (DARWIN EU), EMA’s network of data and services in Europe for a better use of real-world evidence when assessing medicines: the workplan foresees more than one hundred DARWIN EU studies per year by 2025;
- Data quality: a data quality framework for the EU regulatory network is to be delivered by the end of 2022, following the analysis and exchanges on data quality with a wide range of stakeholders including patients, healthcare professionals, regulators, pharmaceutical industry and academia;
- Data discoverability: the workplan foresees the publication of a good practice guide on real-world metadata and a public catalogue of European real-world data. In addition, searching for information from regulatory documents will be enhanced through the development of analytics tools and the development of standardised clinical trial protocols;
- EU network skills: the workplan includes the delivery of training on biostatistics, pharmacoepidemiology and data science for regulators with targeted access for patients, healthcare professionals and academics.
Big data are extremely large, rapidly accumulating datasets captured across multiple settings and devices, for example through wearable devices and electronic health records. Coupled with rapidly developing technology, big data can complement the evidence from clinical trials by filling knowledge gaps on a medicine, and can help to better characterise diseases, treatments and the performance of medicines in individual healthcare systems.
The work carried out by the Big Data Steering Group builds on the Regulatory Science Strategy to 2025, published in March 2020, and will support the European Medicines Agencies Network Strategy to 2025.
HMA/EMA Joint Big Data Steering Group Workplan 2022-2025 | pdf
Contact
Heads of Medicines Agencies Permanent Secretariat
E-mail: ps@hma.eu
European Medicines Agency
Media enquiries
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
All other enquiries
Please submit your request via the online form
Follow us on Twitter @EMA_News
A Big Data strategy for veterinary medicines in the EU
The European Medicines Agency (EMA) and the Heads of Medicines Agencies (HMA) have adopted a Veterinary Big Data strategy to 2027 outlining their vision for the regulation of data-driven, digital innovations in the veterinary medicines’ domain in the EU.
Building upon key objectives of the recently implemented Veterinary Medicinal Products Regulation (Regulation (EU) 2019/6), the strategy proposes concrete steps to converge traditional regulatory practise with innovative digital solutions.
As part of the implementation of the veterinary legislation, EMA and the EU Veterinary Medicines regulatory network have already made significant investments in implementing new IT systems that generate and centrally collect an increased amount of data. The strategy sets up a framework for managing and using these data to support key regulatory activities to enhance consistency, transparency and responsiveness by providing accurate and reliable information to promote public and animal health.
The Veterinary Big Data strategy proposes implementation in phased steps:
- Up to 2023: strengthen collection of key underlying data and identification of additional data sources to better support regulatory activities in subsequent implementation phases
- 2023-2025: integrate key data in targeted regulatory processes and start analytics solutions
- 2024-2027: connect data to power information sharing and dissemination and expand analytic capabilities. The phase will be aligned with the Big Data strategy for human medicines.
It impacts different business areas, such as pharmacovigilance, antimicrobial resistance, environmental risk assessment, regulatory submission, innovation of veterinary medicinal products development, demonstration of efficacy/effectiveness.
This strategy also proposes approaches to identify relevant use cases, existing and additional data sources, critical infrastructures and methods to foster an environment that encourages innovation.
Notes
- This press release, together with all related documents, is available on EMA's website
- The first veterinary big data stakeholders forum took place in June 2021 and a follow-up stakeholder forum will be held on 23 November 2022.
- More information on the work of the European Medicines Agency can be found on its website.
Contact
Heads of Medicines Agencies Permanent Secretariat
E-mail: ps@hma.eu
European Medicines Agency
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Twitter: @EMA_News
CTCG recommendation to sponsors on managing the impact of the war in Ukraine on clinical trials
In view of the specific circumstances linked to the war in Ukraine, the Clinical Trials Coordination Group (CTCG) developed recommendations to sponsors on managing the impact of the war in Ukraine on clinical trials.
CTCG recommendation to sponsors on managing the impact of the war in Ukraine on clinical trials | pdf
Accelerating Clinical Trials in the EU (ACT EU): for better clinical trials that address patients’ needs
Today, the European Commission (EC), the Heads of Medicines Agencies (HMA) and the European Medicines Agency (EMA) have launched an initiative to transform how clinical trials are initiated, designed and run, referred to as Accelerating Clinical Trials in the EU (ACT EU). The aim is to further develop the EU as a focal point for clinical research, further promote the development of high quality, safe and effective medicines, and to better integrate clinical research in the European health system.
Building on the application of the Clinical Trials Regulation and the launch of the Clinical Trials Information System (CTIS) on 31 January 2022, ACT EU will strengthen the European environment for clinical trials, whilst maintaining the high-level of protection of trial participants, data robustness and transparency that EU citizens expect. The ACT EU strategy paper published today lists ten priority actions for 2022/2023, including enabling innovative trial methods, establishing a multi-stakeholder platform, and supporting the modernisation of good clinical practice. Together, they will contribute to achieving the ambitious goals for innovation in clinical trials set out in the European medicines agencies network strategy (EMANS) to 2025 and the European Commission’s Pharmaceutical Strategy.
ACT EU will be co-led by the EC, EMA and the HMA, who have also collaboratively developed the initiative.
The proposal to establish ACT EU was endorsed by HMA in November and by EMA’s Management Board in December 2021. Further information will be made available on EMA and HMA webpages.
Notes
- This press release, together with all related documents, is available here on EMA's website
- More information on the work of the European Medicines Agency can be found on its website
Contacts
European Commission
Stefan de Keersmaecker, Spokesperson, public health and food safety
E-mail: Stefan.DE-KEERSMAECKER@ec.europa.eu
Darragh Cassidy, Press Officer
E-mail: darragh.cassidy@ec.europa.eu
Heads of Medicines Agencies Permanent Secretariat
E-mail: ps@hma.eu
European Medicines Agency Press Office
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Data standardisation strategy
The European medicines regulatory network's data standardisation strategy sets out principles to guide the definition, adoption and implementation of international data standards by the network.
It aims to:
- enable quicker uptake of international data standards across the EU;
- improve data quality;
- enable data linkage and data analysis to support medicine regulation.
- The strategy is a key deliverable of the Big Data Steering Group workplan.
EMA and HMA published the strategy in December 2021 and will maintain it over time to reflect any changing priorities or new requirements.
European Medicines Regulatory Network Data Standardisation Strategy
New HMA PS email address
Starting from January 1, 2021 new email address is ps@hma.eu. Please note, that your email will not be automatically forwarded, thus kindly change HMA PS address on your records and send any communications to the new address after abovementioned date. If you continue to send to the old email address hma-ps@pei.de, your email will either fail to reach us or it will be received with a significant delay. The old addresses will continue to work for a limited period only.
Joint strategy sets direction for EMA and EU medicines regulatory agencies to 2025
EMA and the Heads of Medicines Agencies (HMA) have published their joint strategy for the next five years, following its recent adoption by the HMA and EMA Management Board.
The strategy details how the European medicines regulatory network can continue to enable the supply of safe and effective medicines that meet patients’ needs in the face of challenges posed by ever-accelerating developments in science, medicine, digital technologies, globalisation as well as emerging health threats, such as the COVID-19 pandemic.
"The COVID-19 pandemic has highlighted the pivotal role of medicine regulation for the protection of public health," said Emer Cooke, EMA’s Executive Director. "Lack of availability of medicines, either because they are not marketed or due to supply disruptions, has shown to pose serious threats to patient and animal health, animal disease control programs and sustainable livestock production. This strategy ensures that we join forces across the EU to effect tangible improvements for citizens."
The European medicines agencies network strategy to 2025 outlines six priority areas for the network:
- the availability and accessibility of medicines;
- data analytics, digital tools and digital transformation;
- innovation;
- antimicrobial resistance and other emerging health threats;
- supply chain challenges; and
- the sustainability of the network and operational excellence.
It identifies strategic goals for each of these areas, which will be translated into concrete actions in the detailed work plans of EMA and the national competent authorities in EU Member States in the coming five years. It also considers some of the recent developments related to the COVID-19 pandemic. Further learnings from the pandemic have been incorporated into the strategy and will be taken into account in subsequent work plans on an ongoing basis.
"We must keep pace with societal changes and developments so that we can continue to fulfil our mission successfully, with the most efficient use of the resources and knowledge available to us," said Thomas Senderovitz, Chair of the Heads of Medicines Agencies Management Group. "This strategy document, which is a living document, will help us to work together across the network to achieve this goal."
The joint EMA//HMA strategy was open for public consultation from July to September 2020. The extensive and helpful feedback from the public consultation, which captured input from a full range of stakeholder groups, was carefully analysed and reviewed in order to refine and finalise the strategy. More detail on the comments received and the network’s analysis of these comments is available in a separate document.
The European medicines agencies network strategy was developed in consultation with the European Commission and the key themes are aligned with those covered in the Commission’s Pharmaceutical Strategy that will set the tone of future pharmaceutical policy for human medicines in the EU.
The network will review the strategy after 18 months to consider if the goals and objectives remain appropriate, and to adjust them if necessary, in the light of the changing environment and ongoing engagement with stakeholders.
Notes
- This press release, together with all related documents, is available on EMA's website.
- The development of the European medicines agencies network strategy to 2025 was also informed by EMA’s Regulatory Science Strategy to 2025 which was published in March 2020.
- The key topic areas and challenges identified in the strategy were presented and discussed with patient, consumer and healthcare professional organisations in March 2020 and industry, academia and veterinary stakeholders contributed through a written consultation.
- More information on the work of the European Medicines Agency can be found on its website.
Contacts
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
European Medicines Agency
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Twitter: @EMA_News
HMA/EMA statement on approval of vaccines
Development and deployment of safe and effective vaccines is seen as an essential element in the management and solution of the COVID-19 pandemic. In continuation hereof, the European Medicines Agency (EMA) and Heads of Medicines Agencies (HMA) have prepare a joint statement on how COVID-19 vaccine applications should be assessed.
Read the joint HMA/EMA statement here or on EMA's website.
HMA, EMA and the European Commission working against COVID-19
HMA supports the development and approval of treatments and vaccines to combat coronavirus since the start of the outbreak. Therefore, our colleagues in National Competent Authorities, the European Medicines Agency and the European Commission are working in partnership and contributing their knowledge. Together we support the development and approval of safe and effective COVID-19 vaccines and treatments. Our common goal is to protect the citizens of the EU.1 Find out more on Twitter: #MedicinesAgenciesAgainstCorona
1 All the COVID-19 related information, guidelines and other documents relevant to the European Medicines Regulatory Network can be found on the HMA website in COVID-19 section.
Launch of public consultation on joint network strategy to 2025
EMA and the Heads of Medicines Agencies (HMA) have developed a joint strategy for the next five years that is released for a two-month public consultation today. The draft strategy details how the European medicines agencies’ network can continue to enable the supply of safe and effective medicines that meet patients’ needs in the face of challenges posed by ever-accelerating developments in science, medicine, digital technologies, globalisation as well as emerging health threats, such as the COVID-19 pandemic.
The European Medicines Agencies Network Strategy to 2025, which builds on the HMA/EMA strategy to 2020, outlines six priority areas for the network:
- the availability and accessibility of medicines;
- data analytics, digital tools and digital transformation;
- innovation;
- antimicrobial resistance and other emerging health threats;
- supply chain challenges; and
- the sustainability of the network and operational excellence.
It identifies high-level goals and supporting recommendations for each of these areas, which will guide and shape the detailed work plans of EMA and the national competent authorities in EU Member States in the coming five years.
Input on the draft strategy document is welcome from all stakeholders, including members of the public, until 4 September 2020 via an online questionnaire.
The draft strategy was developed in consultation with the European Commission (EC) and the key themes are aligned with those covered by the EC’s roadmap for a new Pharmaceutical Strategy. It also takes into account some of the recent developments related to the COVID-19 pandemic. Further learnings from the pandemic will be incorporated into the strategy and subsequent work plans on an ongoing basis.
The key topic areas and challenges identified in the strategy were presented and discussed with patient, consumer and healthcare professional organisations in March 2020 and industry, academia and veterinary stakeholders contributed through a written consultation.
The strategy is intended to be a living document which will be periodically reviewed, and detailed actions to implement it will be further developed by EMA and the national authorities in their multi-annual work plans. For most of these actions the work will be shared between national authorities and EMA and will involve close collaboration.
Following the public consultation, comments from stakeholders and the public will be analysed and considered in the final draft of the document.
The strategy will be considered for adoption by the HMA and EMA Management Board towards the end of 2020. A summary of comments will be published at the time of publication of the final strategy.
A short video to highlight the public consultation has also been published.
European medicines agencies network strategy to 2025 released for public consultation can be found here or on EMA's website.
Notes
- This press release, together with all related documents, is available on EMA's website.
- The development of the European Regulatory Network Strategy to 2025 was also informed by the EMA’s Regulatory Science Strategy to 2025 which was published in March 2020.
- More information on the work of the European Medicines Agency can be found on its website.
Contact our press officers
European Medicines Agency
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Follow us on Twitter @EMA_News
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
European regulators make recommendations drawing on lessons learnt from presence of nitrosamines in sartan medicines
The European medicines regulatory network has issued recommendations on impurities in medicines following the conclusion of an exercise to draw on lessons learnt from the presence of nitrosamines in a class of blood pressure medicines known as sartans.
The recommendations aim to clarify the roles and responsibilities of companies involved in the manufacture of medicines and to amend guidance on controlling impurities and good manufacturing practice. The recommendations also cover the management of impurities once detected, communication with patients and healthcare professionals, and international cooperation. The full recommendations are available on EMA’s website.
The network noted that nitrosamines were not previously recognised as potential impurities in sartan medicines, and these recommendations will help both regulators and companies better prevent and mitigate the risks of these and other impurities in the future.
Nitrosamines are classified as probable human carcinogens (substances that could cause cancer) based on animal studies.
Regulators in the EU first became aware that they were present in some sartan medicines in mid-2018. The discovery led to swift regulatory action, including the recall of medicines and measures to stop the use of active substances from certain manufacturers. A subsequent EU review, which concluded in April 2019, established the sources of nitrosamines and set out new manufacturing requirements for sartans.
Although the exercise focused on nitrosamines in sartans, the recommendations will help reduce the risk of impurities being present in other medicines and ensure that regulators are better prepared to manage cases of unexpected impurities in the future.
In September 2019, EMA launched an Article 5(3) procedure to provide additional guidance to companies that make and market medicines in the EU. The recommendations of the lessons learnt exercise will complement the outcome of this Art 5(3) procedure which will provide the key scientific opinion on the presence of nitrosamine impurities in human medicines containing chemically synthesised active substances.
Reviewing practices on the basis of experience is one of the ways the authorities in the EU ensure that medicines in the EU are of the highest quality. EU authorities will continue working closely with the European Directorate for the Quality of Medicines & HealthCare and international partners and will take necessary measures to protect and reassure patients.
European medicines regulatory network fully mobilised in fight against COVID-19
The development and availability of medicines and vaccines for all patients in the European Union, including those with COVID-19, is the number one priority for the European medicines regulatory network. EMA, together with EU Member States and the European Commission, has published a plan outlining principles for how the network will ensure that core public and animal health regulatory activities, such as the authorisation, maintenance and supervision of human and veterinary medicines will continue to be carried out during the ongoing COVID-19 pandemic.
This includes, in the first instance, procedures related to potential treatments for COVID-19 and vaccines against the virus, those related to medicines needed to treat COVID-19 patients (including crucial medicines used in intensive care units) and procedures to minimise shortages due to COVID-19. The plan also ensures that the EU regulatory system continues to address all other patients’ needs. It therefore sets out how the assessment of non-COVID-19-related medicines will be undertaken during the COVID-19 pandemic, especially when challenges are encountered, for example, with the unavailability of experts due to illness or the need to look after family members.
The plan aims to support the continued functioning of the network as a whole through a consistent approach for all medicines, irrespective of whether they are centrally or nationally authorised.
It includes how Member States could provide back-up for each other, if the disruptions caused by COVID-19 affects their ability to carry out assigned assessments.
Under no circumstances can the assessment of medicines used to treat or prevent COVID-19 be delayed, and Member States must consider their resources and capacity, when putting themselves forward to deal with such an assessment on behalf of the EU.
Delays to the assessment of non-COVID-19-related medicines must also be mitigated as far as possible. Should delays occur for a non-COVID-19 procedure, these will be dealt with according to the details set out in the annexes. Details for medicines subject to the centralised authorisation procedure are outlined in Annex 1 of the document. Arrangements for nationally authorised human medicines are described in Annex 2 and those specific to nationally authorised veterinary medicines are outlined in Annex 3.
More details are provided in the plan, which will be reviewed regularly and revised as needed. EMA and the network will provide further updates and guidance on its implementation as necessary.
Notes
1. This press release, together with all related documents, is available on EMA's website.
2. The European medicines regulatory network is the network of national competent authorities of the EU Member States, and of the European Economic Area (EEA) working together with EMA and the European Commission.
3. More information on the work of the European Medicines Agency can be found on its website: www.ema.europa.eu
Contact our press officers
European Medicines Agency
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Follow us on Twitter @EMA_News
European Commission
Stefan de Keersmaecker, Spokesperson public health and food safety
E-mail: Stefan.DE-KEERSMAECKER@ec.europa.eu
Darragh Cassidy, press officer
E-mail: darragh.cassidy@ec.europa.eu
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
Questions and answers on regulatory expectations for medicinal products for human use during the COVID-19 pandemic
The European Commission, the Coordination group for Mutual recognition and Decentralised procedures – human (CMDh) and the European Medicines Agency (EMA) have developed a Questions and answers document on regulatory expectations for medicinal products for human use during the COVID-19 pandemic.
The current COVID-19 pandemic has a considerable impact on citizens, patients and businesses. It may force MAHs and regulatory authorities to operate under business continuity mode, impacting the standard way of working. Moreover, public health needs may require quick actions or re-prioritisation of operations.
The ultimate aim of the EU legislation on medicinal products is to ensure a high level of public health. The COVID-19 pandemic is posing unprecedented challenges and ensuring continuity of supplies of medicines is a priority for public health. Therefore, it is necessary to articulate appropriate measures to minimise risks of shortages while ensuring that the high standards of quality, safety and efficacy of medicines made available to patients in the EU are maintained.
This document provides guidance to marketing authorisation holders of medicinal products for human use (MAHs) on regulatory expectations and flexibility during the COVID-19 pandemic. The document will be updated to address new questions and to adjust the content thereof to the evolution of the pandemic. For queries related to specific products that are not specifically addressed in this document, MAHs are invited to address the EMA (for centrally authorised products) or the relevant national competent authorities (for nationally authorised products).
Guidance to sponsors on how to manage clinical trials during the COVID-19 pandemic
The European Commission, the European Medicines Agency (EMA) and national Head of Medicines Agencies (HMA) have published new recommendations for sponsors on how to manage the conduct of clinical trials in the context of the coronavirus disease (COVID-19) pandemic. The impact of the pandemic on European health systems and more broadly on society, will make it necessary for sponsors to adjust how they manage clinical trials and the people who participate in these trials.
The guidance provides concrete information on changes and protocol deviations which may be needed in the conduct of clinical trials to deal with extraordinary situations, e.g. if trial participants need to be in self-isolation or quarantine, access to public places (including hospitals) is limited due to the risk of spreading infections, and healthcare professionals are being reallocated.
This guidance includes a harmonised set of recommendations, to ensure the utmost safety of trial participants across the European Union while preserving the quality of the data generated by the trials. It also advises how these changes should be communicated to authorities.
There is specific advice on the initiation of new clinical trials for treatments of COVID-19, and in particular on the need for large, multinational trial protocols. This is in line with the call issued on Thursday by EMA’s human medicines committee (CHMP) for robust trial methodology in clinical trials for potential COVID-19 treatments or vaccines.
The guidance was agreed by the Clinical Trials Expert Group (CTEG) of the European Commission supported by EMA, the Clinical Trials Facilitation and Coordination Group (CTFG) of HMA and the GCP Inspectors’ Working Group. It provides a harmonised approach in the conduct of trials, in order to mitigate the negative effects of the pandemic.
In the EU, clinical trials are authorised and supervised at national level. Sponsors are advised to also check whether there might be specific national legislation and guidance in place to complement or in some cases to take priority over this new guidance.
Notes
- The guidance on the management of clinical trials during COVID-19 is published on the European Commission’s website.
- For more information on the EU’s response on coronavirus 2019-nCoV, see European Commission: Coronavirus response.
- More information about EMA’s response to COVID-19 is available here.
- More information about the CTFG is available here.
- Information on the GCP Inspector’s working group is available here.
- Information on the CTEG (Clinical Trials Expert Group) is available here.
Contact our press officers
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
EMA press office
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
European Commission
Stefan de Keersmaecker, Spokesperson public health and food safety
E-mail: Stefan.DE-KEERSMAECKER@ec.europa.eu
Darragh Cassidy, press officer
E-mail: darragh.cassidy@ec.europa.eu
Updated - European authorities working to avoid shortages of medicines due to Brexit – questions and answers
Updated version of the document "European authorities working to avoid shortages of medicines due to Brexit – questions and answers" has been prepared by the European Medicines Agency (EMA).
The document provides answers to potential questions on the supply of medicines in the EU in the context of Brexit. Likewise, it explains what EMA, the European Commission and national competent authorities in the Member States are doing to prevent potential medicine supply shortages due to Brexit.
"European authorities working to avoid shortages of medicines due to Brexit – questions and answers"
The EU-Innovation Network (EU-IN) announces the introduction of a pilot for Simultaneous National Scientific Advice (SNSA)
The EU-Innovation Network (EU-IN) announces the introduction of a pilot for Simultaneous National Scientific Advice (SNSA) to further strengthen early regulatory support for innovation, featuring:
- Coordinated approach to different National Competent Authorities (NCAs), providing broader expertise for a defined set of questions and data package in line with the procedure for national scientific advice (e.g. minutes and fees)
- Opportunity to discuss issues early and simultaneously across selected Member States
- Possibility to achieve consolidated views and identify divergent opinions of the participating NCAs
- Supporting measure to encounter the timelines of the new clinical trial regulation
- Tool for early identification of critical scientific or regulatory issues that may require formal EU scientific advice at EMA
- Discussion of the experience and learnings from completed SNSA cases at the EU-IN and potentially relevant working groups and scientific committees of EMA, to support knowledge sharing within the regulatory network, to enhance preparedness for incoming innovation and reflect on regulatory challenges
Start of the pilot to develop a best practice model is February 1st, 2020 with as many different NCA pairs as possible and potential extension planned to the participation of more than two NCAs beyond 2020 pending on a positive outcome of the pilot evaluation at the end of 2020.
Guidance for applicants on a pilot for SNSA
Key principles for the use of electronic product information for EU medicines
EMA, the Heads of Medicines Agencies (HMA) of EU Member States and the European Commission (EC) have published today key principles outlining a harmonised approach to develop and use electronic product information (ePI) for human medicines across the European Union.
The product information (PI) of a medicine includes the package leaflet for patients and the summary of product characteristics (SmPC) for healthcare professionals. These documents accompany every single medicine authorised in the EU and explain how it should be prescribed and used. The package leaflet is provided in the medicine’s box and can also be found, often as a pdf document, on the websites of EU regulators. However, digital platforms open additional possibilities to disseminate the PI electronically. This can address some of the current limitations (e.g. the current PI is not interoperable with other electronic health systems such as e-prescription and electronic health records) and better meet patients’ and healthcare professionals’ needs for accessible, trustworthy and up-to-date information on medicines available at the right time.
The ePI initiative was launched to support the digital transformation of healthcare across the EU, and the commitment laid out by the European Commission to prioritise innovations that will empower citizens and build a healthier society. It is also in line with EMA’s current digitalisation efforts aiming to make best use of available resources and prepare for future challenges.
The key principles describe the benefits ePI can deliver for public health and the efficiencies it may introduce in regulatory procedures. They explain how ePI will be provided as open access information that complements the paper package leaflet. They also outline a flexible, harmonised approach to implementation across the EU, and describe how ePI will work in the EU’s multilingual environment and will interact with other ongoing digital initiatives at EU and global level.
The key principles derive from extensive discussions and consultations carried out in 2018 and 2019 by EMA, HMA and the EC with representatives of all stakeholder groups concerned, from patients, healthcare professionals and regulators to the pharmaceutical industry. In particular, during a public consultation that took place from January to July 2019, 71 contributions from all stakeholder groups were received, including over 500 comments which were considered for the final version. A summary of the main points raised in the consultation and the submissions are also published today.
The key principles were endorsed at the end of 2019 by EMA’s Management Board and by the HMA. They are now expected to be followed by all parties involved in the process of developing and implementing ePI for medicines across the EU.
Notes:
1 Document "Key principles outlining a harmonised approach to develop and use electronic product information (ePI) for human medicines across the European Union" and related documents are available at EMA's website.
Contact points:
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail:ps@hma.eu
EMA press office
Tel. +44 (0)20 3660 8427
E-mail: press@ema.europa.eu
European Commission
Vivian Loonela, Spokesperson public health and food safety
E-mail: vivian.loonela@ec.europa.eu
Darragh Cassidy, press officer
E-mail: darragh.cassidy@ec.europa.eu
Ten recommendations to unlock the potential of big data for public health in the EU
The joint Big Data Task Force of EMA and the Heads of Medicines Agencies (HMA) proposes ten priority actions for the European medicines regulatory network to evolve its approach to data use and evidence generation, in order to make best use of big data to support innovation and public health, in a report published today.
Big data are extremely large, rapidly accumulating datasets captured across multiple settings and devices, for example through wearable devices, electronic health records, clinical trials or spontaneous adverse reaction reports. Coupled to rapidly developing technology, big data can complement the evidence from clinical trials and fill knowledge gaps on a medicine, and help to better characterise diseases, treatments and the performance of medicines in individual healthcare systems. The rapidly changing data landscape forces regulators to evolve and change the way they access, manage and analyse data and to keep pace with the rapid advances in science and technology.
“I look forward to working with the European Commission and national competent authorities to see how these concrete proposals can be implemented to better harness the potential of big data. This will help to further strengthen the robustness and quality of the evidence upon which we take decisions on medicines,” said Guido Rasi, EMA’s Executive Director.
“The changes proposed will require investment to build up capacity and skills at national and EU level. This is needed if we want to establish the EU network as a reference for data-driven decision-making,” said Thomas Senderovitz, Chair of the HMA Management Group.
The report makes several recommendations out of which ten are viewed as priorities. The most ambitious of these top ten recommendations is the establishment of an EU platform to access and analyse healthcare data from across the European Union (Data Analysis and Real World Interrogation Network, or DARWIN). This platform would create a European network of databases of verified quality and content with the highest levels of data security. It would be used to inform regulatory decision-making with robust evidence from healthcare practice.
Other recommendations are intended to enhance guidance and resources within the EU regulatory network for data quality and data discoverability (choice of key metadata) and to build up computing and analytical capacity. The joint task force advises to develop the skills to process and analyse big data within the network through training to enhance the capacity of regulators to assess applications for the authorisation of medicines that use big data sources as part of the evidence on benefits and risks. It proposes to establish a learning initiative to track and review outcomes of these types of submissions.
The report also emphasises the need to ensure data are managed and analysed within a secure and ethical governance framework, and in active dialogue with key EU stakeholders including patients, healthcare professionals, industry, Health-Technology Assessment bodies (HTAs), payers, device regulators and technology companies. All these activities should be done in collaboration with international initiatives on big data.
Established in 2017, the HMA - EMA Joint Big Data task force is composed of experienced medicines regulators and data experts appointed by national competent authorities, EMA and the European Commission. The first phase of its work -published in early 2019- reviewed the landscape of big data and identified opportunities for improvements in the operation of medicines regulation. Published today, the practical suggestions made in the second phase of its work aim to inform strategic decision-making and planning by the HMA and EMA and to contribute to the upcoming EU Network Strategy to 2025. The implementation of the recommendations is being considered in full consultation with the European Commission services.
Notes
- This press release, together with all related documents, is available on the two agencies’ websites.
- More information on big data in medicines’ regulation and the HMA/EMA Task force on big data is available here.
Contact points
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
EMA press office
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Medicine shortages: EU network takes steps to improve reporting and communication
The EU task force set up to address problems with medicines supply has published two documents today:
- Guidance for marketing authorisation holders on reporting of shortages in the EU
- Good practice guidance for communication to the public on medicines’ availability issues.
The task force was established by European Union regulators to better address potential problems with medicines’ supply and to develop and coordinate actions to facilitate the prevention, identification, management of and communication about shortages.
Both documents lay the foundations for an improved and harmonised EU approach in reporting of and communication on medicines’ shortages and availability issues, a key public health priority for the EU network.
The first document provides guidance to the pharmaceutical industry, a key player in addressing shortages, to facilitate the detection and early notification to competent authorities. The guidance is based on a common definition of the term "shortages", which should enable a more harmonised and timely approach in the detection and management of issues with the supply of medicines. A proposed template for shortage notification by companies is included in the guidance. The guidance and template will be implemented in a pilot phase, which is currently planned to start in the last quarter of 2019. Further information will be provided nearer the time.
The second document, addressed to EU national competent authorities and EMA, lays out principles and examples of good practices for communication on shortages to the public, including patients and healthcare professionals. These groups require timely, accurate and up-to-date information on availability issues to ensure continuity of care. The guidance is based on a survey carried out by the task force in all EU Member States to collect information on how issues related to shortages and availability of medicines are measured and communicated to the public.
The documents are two key deliverables of the task force and they have undergone extensive consultation with stakeholder groups, including at a multi-stakeholder workshop in November 2018. They are listed in the work programme 2018-2020, which has been recently updated.
The task force was set up by the European Medicines Agency (EMA) and the Heads of Medicines Agencies (HMA), with representatives from the European Commission and national competent authorities, the chairs of the Co-ordination Group for Mutual Recognition and Decentralised Procedures – Human (CMDh) and Veterinary (CMDv), the GMP/GDP Inspectors Working Group, the Working Group of Communication Professionals (WGCP) and the European Surveillance Strategy Working Group (ESS WG).
Shortages and availability problems are complex with no quick solutions. Medicine regulatory authorities are only one of the many actors involved in availability issues, however they play an important role in prevention and management. By bringing together experts from various EU member states, the work of the task force lays the foundations for an improved and harmonised EU approach in addressing the problems of medicines’ availability issues. Its mission is to develop and coordinate actions for better prevention, identification, management of and communication on issues that can affect the availability of medicines, in order to improve continuity of supply of human and veterinary medicines across Europe.
Notes
1. The updated work programme and the two guidance documents are available on the websites of both EMA and HMA.
Contact points:
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
EMA press office
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Call for all sponsors to publish clinical trial results in EU database
The European Commission (EC), the European Medicines Agency (EMA) and the Heads of Medicines Agencies (HMA) have co-signed a letter reminding all sponsors of clinical trials conducted in the European Union of their obligation to make summaries of results of concluded trials publicly available in the EU Clinical Trials Database.
Transparency and public access to clinical trial results, whether positive or negative, are fundamental for the protection and promotion of public health. It assures trial subjects that their voluntary participation in clinical trials is useful and that the results have been collated and reported for the benefit of all. In addition for those medicines which are placed on the market or used in further clinical trials it allows patients and healthcare professionals, or any other citizen, to find out more information about medicines they might be taking or prescribing. Transparency also enhances scientific knowledge, and helps to advance clinical research and support more efficient medicine development programmes.
It is the responsibility of sponsors to ensure that the protocol information and results of all clinical trials is submitted in the EU Clinical Trials Database (EudraCT); this information is publicly available through the EU Clinical Trials Register (EU CTR). Since July 2014, sponsors are required to post results within one year after the end of a clinical trial (or 6 months for a paediatric trial). This information is also shared with the World Health Organization’s (WHO) International Clinical Trials Registry Platform (ICTRP) of which EU CTR is a primary registry.
As of April 2019, the EudraCT database included 57,687 clinical trials in total, out of which 27,093 were completed. Out of these completed trials, 18,432 should have had results posted; sponsors were in compliance of the publication requirements for 68.2% (12,577) of the trials, however results were still lacking for 31.8% of them (5,855).
The reporting compliance of non-commercial sponsors (e.g. academia) was much lower than for commercial sponsors (i.e. companies), with 23.6% of results posted for non-commercial sponsors vs 77.2% for commercial sponsors. Academic sponsors or smaller companies often lack awareness or incentives to post clinical results, therefore the EU authorities are taking various steps to ensure sponsors are aware of their obligations and can act on them.
One of these initiatives is the "letter to stakeholders regarding the requirements to provide results for authorised clinical trials in EudraCT", co-signed by Anne Bucher, Director General of the EC’s DG Health and Food Safety, Guido Rasi, Executive Director of EMA, and Thomas Senderovitz, Chair of HMA Management Group. It will be disseminated to various stakeholder groups, with a goal in particular to reach academic sponsors. This should help to spread the word about the importance of making clinical trial results publicly available.
Amongst other initiatives conducted at EU level, EMA has since September 2018 been identifying trials with missing results on a monthly basis and sending reminders to the sponsors of those trials to ensure compliance with the transparency rules and their follow up on their results reporting obligations.
Contact points:
European Commission
Anca Paduraru, Spokesperson public health and food safety
Tel. +32 2 299 12 69
E-mail: anca.paduraru@ec.europa.eu
EMA press office
Tel. +31 (0)88 781 8427
E-mail: press@ema.europa.eu
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
HMA - EMA Joint Big Data Task Force Summary Report and public consultation on core recommendations
Recommendations for a path towards understanding the acceptability of evidence derived from ‘big data’ in support of the evaluation and supervision of medicines by regulators were published today as part of a summary report of the HMA (Heads of Medicines Agencies) -EMA Joint Big Data task force. The recommendations and associated actions set out what needs to be addressed, but the mechanisms by which this may be achieved requires further focussed work over the coming year. Stakeholders are invited to submit feedback and observations on the recommendations to inform the upcoming work of the group.
Massive amounts of data are generated on a daily basis through wearable devices, electronic health records, social media, clinical trials or spontaneous adverse reaction reports. There is no doubt that insights derived from this data will increasingly be used by regulators to assess the benefit-risk of medicines across their whole lifecycle. However, in order to benefit from and make prudent use of the data collected, regulators need a deeper understanding of the data landscape.
The HMA - EMA Joint Big Data task force is composed of experienced medicines regulators from 14 national competent authorities and EMA. In preparing the report, it assessed the generation of ‘big data’, their relevant sources and main formats, the methods for processing and analysing big data and the current state of expertise across the European medicines regulatory network.
A crucial step was defining ‘big data’ itself, a widely used term that is lacking a commonly accepted definition. The definition adopted by the task force reads as follows: “extremely large datasets which may be complex, multi-dimensional, unstructured and heterogeneous, which are accumulating rapidly and which may be analysed computationally to reveal patterns, trends, and associations. In general, big data sets require advanced or specialised methods to provide an answer within reliable constraints.”
Six subgroups of data sources relevant to regulatory decision making were considered by the taskforce: genomics, bioanalytical ‘omics (proteomics, etc.), clinical trials, observational data, spontaneous adverse drug reactions data and social media and mobile health data.
Stakeholders and members of the public are invited to submit their comments on the core recommendations in the summary report (not to exceed 1,000 words) to Bigdatasec@dkma.dk until 15 April 2019. In particular, views on prioritisation of future actions would be welcomed. The feedback received will be taken into account in the next phase of the work of the task force. A newly refined mandate for the group is in place for the next year to define next steps and prioritisation of actions.
HMA contact:
Heads of Medicines Agencies Permanent Secretariat
c/o Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen
Germany
E-mail: ps@hma.eu
Withdrawal of the UK and EU rules for Quality testing of medicinal products
Letter of European Commission | pdf, 21 February 2019
Towards electronic product information for EU medicines
EMA, the Heads of Medicines Agencies (HMA) and the European Commission (EC) are organising a workshop on 28 November 2018 in London to agree with various stakeholders on common EU key principles to pave the way for implementing electronic product information (ePI) in the EU.
The product information (PI) of a medicine in the EU includes the package leaflet for patients and the summary of product characteristics (SmPC) for healthcare professionals. These documents accompany every single medicine authorised in the EU and explain how it should be used and prescribed.
The workshop follows up on an EC report highlighting that, despite efforts to make the PI easy to read and useful, there is still a need to improve how information on medicines is conveyed to patients and healthcare professionals.
One of the key areas of this report is to explore how electronic formats can be used to improve citizens’ access to medicines' information. The package leaflet is currently provided in the medicine’s box and can also be found, mainly as a pdf document, on the regulators’ website. However, novel digital platforms open additional possibilities to disseminate the package leaflet electronically. This can enhance access to up-to-date information and offer new opportunities to better tailor this information to the needs of patients. In addition, ePI will support patients with visual impairments and citizens with low literacy levels.
The workshop offers a platform for healthcare professionals, patients and consumers, academics, non-profit organisations, regulators and the pharmaceutical industry to discuss:
- opportunities, needs and concerns identified by different stakeholder groups;
- ongoing initiatives in the EU;
- how ePI fits into other EU and global initiatives.
The outcome of the workshop will serve as a basis to draft key principles for the use of ePI in the EU, which will be released for a six-month public consultation in January 2019.
The workshop will be live streamed on EMA’s website. No registration or password is required. Participants interested in tweeting about this event are invited to use the hashtag #ePI4Medicines.
Progress on using electronic means for a better dissemination of product information in Europe is one of the key priorities of the action plan that EMA published in 2017 to address the shortcomings identified in the EC report and to improve the PI for EU medicines. In addition to electronic formats for the PI, other initiatives focus on:
- how to make the package leaflet easier to understand for EU citizens;
- strengthening patients' input during the preparation of the package leaflet;
- updating the EU guidance and sharing best practices on preparing the package leaflet.
The timelines of these activities may need to be adjusted in view of EMA's business continuity plan in the context of Brexit and the Agency's upcoming relocation to the Netherlands. EMA and the European Commission are committed to working together with EU Member States to successfully implement the action plan. All relevant stakeholders will be involved as their input is crucial to ensure that their needs are addressed.
Contact our press officers
European Commission
Anca Paduraru, Spokesperson public health and food safety
Tel. +32 2 299 12 69
E-mail: anca.paduraru@ec.europa.eu
EMA press office
Tel. +44 (0)20 3660 8427
E-mail: press@ema.europa.eu
Heads of Medicines Agencies Permanent Secretariat
Paul-Ehrlich-Institute
Paul-Ehrlich-Straße 51-59
63225 Langen Germany
E-mail: ps@hma.eu
Working with stakeholders to improve availability of medicines in the EU
The Task Forceset up by EMA and the Heads of Medicines Agencies (HMA) on availability of authorised human and veterinary medicines is organising a two day-workshop (8-9 November 2018) at EMA in London to gather stakeholders' perspectives on how to better address potential problems with the supply of medicines and how to avoid shortages of medicines.
Improving the availability of human and veterinary medicines authorised in the EU is a key priority of the EU Medicines Regulatory Network. The aim of the Task Force is to develop and coordinate actions for better prevention, identification, management of and communication on issues that can affect availability of medicines, in order to improve continuity of supply of human and veterinary medicines across Europe. In the context of the potential supply disruption of medicines following the UK’s withdrawal from the EU, the Task Force is serving as a platform to facilitate and coordinate actions between Member States, EMA and the European Commission.
The Task Force’s work programme for the coming two years was published in August 2018.
Day 1 of the workshop is a technical meeting with industry stakeholders to focus on the pharmaceutical industry’s critical role in the prevention and management of medicine shortages. Industry stakeholders are invited to give their feedback on the technical implications of some of the actions set out in the work plan of the Task Force in the field of human medicines and to present best practices already developed for the prevention of shortages.
Day 2 of the workshop will bring together regulators, industry representatives, healthcare professionals, patients and consumers, academia and NGOs. The purpose of this second day is to obtain the views of all stakeholders on the work of the Task Force and to discuss how the different stakeholder groups can contribute to the actions in the workplan. The workshop will mainly focus on human medicines; however, issues common to both human and veterinary medicines will be addressed in the context of Brexit.
The workshop is by invitation only but day 2 will be broadcast live on EMA’s website. Link to live broadcast of the HMA/EMA multi-stakeholders workshop on 9 November can be found here.
Agendas for both days are available.
The Task Force consists of representatives from EMA, the European Commission and National Competent Authorities, the chairs of the Co-ordination Groups for Mutual Recognition and Decentralised Procedures – Human (CMDh) and Veterinary (CMDv), the GMP/GDP Inspectors Working Group, the HMA Working Group of Communication Professionals (WGCP) and the European Surveillance Strategy Working Group (ESS WG).
Safety features implementation
The delegated Regulation on the characteristics of the safety features and the new medicine verification system will apply as of 9 February 2019. More information for the Marketing Authorisation holders, wholesalers or pharmacies can be found on the attached joint letter drafted by DG Santé, HMA and EMA.
The European Commission currently do not plan to exempt additional prescription medicines or product categories from the requirements to bear features ("whitelisting"). All stakeholders must be ready to meet their obligations on 9 February 2019.
For further details please see the European Commisssion website
Towards improving the availability of medicines in the EU
The Task Force set up by European Union (EU) regulators to better address potential problems with medicines’ supply and to avoid shortages published today its work programme for the coming two years. Improving the availability of human and veterinary medicines authorised in the EU is a key priority of the EU Network. The work programme lists actions for regulators and industry alike to ensure the availability of medicines for the benefit of patients in the EU.
The Task Force has been set up by the Heads of Medicines Agencies (HMA) and the European Medicines Agency (EMA) with representatives from the European Commission and interested national competent authorities, the chairs of the Co-ordination Group for Mutual Recognition and Decentralised Procedures – Human (CMDh) and Veterinary (CMDv), the GMP/GDP Inspectors Working Group, the Working Group of Communication Professionals (WGCP) and the European Surveillance Strategy Working Group (ESS WG).
The Task Force will develop and coordinate actions for better prevention, identification, management of and communication on issues that can affect the availability of medicines, in order to improve continuity of supply of human and veterinary medicines across Europe.
Key priorities of the Task Force include:
- Looking at ways to minimise supply disruptions and avoid shortages by facilitating approval and marketing of medicines using the existing regulatory framework (e.g. using work sharing and reduced timetables when possible);
- Developing strategies to improve prevention and management of shortages caused by disruptions in the supply chain (e.g. developing guidance for companies on reporting of shortages);
- Encouraging best practices within industry to prevent shortages;
- Improving sharing of information and best practices among EU regulatory authorities to better coordinate actions across the EU;
- Fostering collaboration with stakeholders and enhancing communication of supply problems to EU citizens.
The Task Force will organise a multi-stakeholder workshop on 8-9 November 2018 to gather stakeholders’ perspectives on how to address availability issues and to include their input into the deliverables of the task force. It will bring together all stakeholders impacted, including patients, consumers, healthcare professionals, industry, wholesalers/distributors, parallel distributors, academia and regulators.
The withdrawal of the United Kingdom from the EU is also likely to affect the availability of medicines in the EU. In this context, the Task Force provides a platform to facilitate and coordinate actions between Member States, EMA and the European Commission.
Work programme of the HMA/EMA task force on availability of authorised medicines for human and veterinary use | pdf
EU regulatory network reflection paper on the availability of authorised medicinal products for human and veterinary use | pdf
EMA goes to: Amsterdam – congratulations from the Heads of Medicines Agencies!
The decision for the new EMA location has been made: Amsterdam will be the future home of the European Medicines Agency (EMA). The Heads of Medicines Agencies (HMA) compliment The Netherlands on this extraordinary success.
"The Amsterdam location will allow the experts from the national European agencies regulating medicines in Europe to travel to EMA and continue their important work in the EMA committees and working parties” says Prof. Cichutek, chair of the HMA Management Group.
The EMA’s business procedures are crucial for the continued efficient coordination of the centralized work of the European Medicines Competent Authorities. A timely and smooth relocation is an important prerequisite. This ensures that the experts of the European medicines agencies are able to access the EMA continuously and easily allowing them to maintain and promote regulation of safe and efficacious medicines for European patients.
Big Data Industry Stakeholder Survey
Rapid developments in technology have resulted in the generation of vast volumes of data, creating new evidence, which has the potential to add significantly to the way benefit-risk of medicinal products is assessed over their entire life cycle. While creating huge opportunities, it is recognised that there are also significant challenges in the use of these data. The HMA/EMA Joint Task Force on Big Data was launched in March of this year as an initial response to these challenges.
As part of its work, the Task Force launches an e-survey addressed to pharmaceutical companies to inform the development of a Big Data Strategy for the European Medicines Regulatory Network. The survey seeks to understand the current experience, key challenges, applicability and added value of Big Data in the context of the life cycle of a product.
The e-survey can be found here
The questionnaire is open until 20 October 2017. A summary report will be made publically available as an output of the Task Force. For queries on the survey, please write to tse@dkma.dk.
Veterinary stakeholders meeting: Lumpy skin disease
A Stakeholder focus group meeting on availability of Lumpy Skin Disease (LSD) vaccines attended by all National Competent Authorities was held in London on January 31, 2017.
There was an unequivocal preference by all stakeholders, notably National Competent Authorities, farmers and consumers, to have access to vaccines manufactured and tested to EU standards to guarantee the quality, safety and efficacy of products used on the territories. The objectives of the meeting were to assess the situation with regard to the currently available vaccines, and to identify steps that could facilitate the authorisation of LSD vaccines to EU standards.
Causes of Lumpy skin disease
Lumpy skin disease is caused by a Capripoxvirus affecting cattle, but showing specific characteristics when compared to Sheepoxvirus and Goatpoxvirus. The mechanism for virus transmission is still unclear, but mosquitoes and flies seem to play an important role as mechanical vectors. The disease was first identified in Zambia in 1929, and moved subsequently to the southern part of Africa, then spread north through Africa before reaching Israel in 1989. It is now endemic in Turkey and it reached Greece in 2015 and Bulgaria in 2016. These two member states started vaccination under Article 8 of Directive 2001/82/EC with non-EU authorized vaccines, in 2015 and 2016 respectively. Although not yet infected, Croatia started also vaccination because it is neighboring the infected areas.
Lumpy skin disease signs range from inapparent to severe disease, including fever, discharge from the eyes and nose, nodular, necrotic skin lesions, edema of the limbs, and swollen lymph nodes. Morbidity can be very high (up to 45%) but mortality is moderate (up to 10%). LSD is of economic importance, due to weight loss, drop in milk production, less frequently abortion and death.
There are currently no approved vaccines available in the EU for prevention of LSD despite incursion of disease into some MSs since 2015. Under emergency procedures, live homologous attenuated vaccines sourced from third regions had been used in MSs to control outbreaks of the disease under the emergency provision of Article 8 of EU Directive 2001/82/EC, based on published data indicating that vaccination can have a significant impact in reducing LSD virus spread and thereby reduce the extent of culling and improve the situation for animal health and welfare.
Preventive measures to avoid Lumpy skin disease
In this context, the feedbacks after vaccination indicated that, although the preventive measures have been effective to limit spreading of the disease, the side effects should not be underestimated: amongst the most serious ones, it appears that the currently available vaccines can cause increased morbidity and mortality of cattle and significant reduction in milk production. It was also highlighted that the clinical diagnosis of LSD is often difficult to achieve, amongst others because the appropriate diagnostic tools are not available.
With regard to the development of vaccines compliant with the EU standard levels, the focus group meeting highlighted major issues from a scientific point of view. As the basic knowledge on the virus and the disease is still incomplete, the development of vaccines is quite challenging; in particular, the morbidity and the mortality rates being low, the number of animals to be included in efficacy trials must be high to hope seeing any benefit from vaccination, and to establish onset and duration of immunity; and finally, even if the reduction in clinical signs might be beneficial for vaccinated animals, another important point would be to prevent spreading of the disease, or at least strongly limiting it. All these aspects have a deep impact on the choice of the vaccine strain and the vaccine formulation.
It was also recognised that more effective collaboration between EU competent authorities and stakeholders is paramount. The French Agency for Veterinary Medicines underlined that EU regulators and animal health risk managers need to understand product development challenges, manufacturing issues (particularly GMP requirements and capacity constraints) and supply time-lines to meet customer expectations. To facilitate the development of vaccines to EU standards, a shared approach for the risks would encourage manufacturers to invest in the development of products for which the potential market was uncertain and unpredictable.
BREXIT
Following the outcome of the UK European Union membership referendum in June 2016 the HMA will have to prepare for the UK leaving the EU. The British regulatory authorities (both MHRA and VMD) expressed and demonstrated that they are committed to the work in the EU medicines regulatory network as long as it remains unclear which changeswillbe implemented. However, the United Kingdom has invoked Article 50, thereby effectuating Brexit, on 29 March 2019.
The European Union has set terms for the negotiation during a Brexit-summit on 29 April 2017. The decision of the UK to leave the EU and the negotiations in the Council lead to uncertainties within the European Medicinal Regulatory Network. To ensure business continuity in case the UK cannot continue to carry out European regulatory procedures, changes in the assignment of MRP/DCP and Centralised Procedures could be implemented in the future.
The HMA and the consequences of the UK leaving the EU
During the HMA meeting on 11 and 12 May 2017 in Valetta during the Maltese EU Presidency all heads agreed to:
1. In cooperation with the EMA continuously supervise HMA and EMA actions in order to avoid any duplications of work.
2. Focus primarily on continuity of DCP/MRP procedures and reply on the EMA with regards to the centralised procedures.
3. Closely cooperate with CMDh, CMDv, Clinical Trial Facilitation Group and all other HMA working groups to ensure the best preperation for the UK leaving the EU. In doing so, to use the analysis and proposals presented in the draft CMD White Papers on Brexit and to invite other HMA groups if relevant to present a similar analysis.
The HMA agreed to set up a Brexit Preparedness working group that will keep oversight of all consequences of Brexit for the workload of the EU medicines regulatory network (the Network) within a preventive manner.
The heads reiterates the wish to have the UK as a close partner in the future and continue the collaboration with the MHRA and VMD.
Worksharing in the Active Substance Master File (ASMF) Assessment
In 2011, the HMA endorsed an idea to use worksharing in the assessment of the Active Substance Master File (ASMF) for multiple procedures. The idea was to save resources and increase consistency in procedures, as the same ASMF was used in different applications for marketing authorisation and was likely to be assessed repeatedly by different assessors. During previous 6 years, the Working Group On Active Substance Master File Procedures has invested a lot of work in the preparation and execution of a worksharing pilot (e.g. updates of existing guidelines, updated assessment report templates, development of ASMF AR database in CTS, development of an EU numbering system, training material for agencies and industry).
As the pilot was successfully finalised, the Heads agreed during the HMA Meeting held in Malta on 23 February 2017 that the ASMF worksharing procedure is a standard procedure to be used. The worksharing procedure is a voluntary option for the industry. In addition, CMDh has been asked to prepare a draft paper with proposals in the direction of an independent assessment of an ASMF as a self-standing procedure and including postmarketing aspects in the further development of an ASMF.
1000th Procedure HMA Voluntary Harmonisation Procedure (VHP) for clinical trials
The European Voluntary Harmonisation Procedure for clinical trials (VHP) was first established in March 2009. Now, the 1000th application for the evaluation of a clinical trial has been received by several European countries. The VHP procedure fosters simultaneous initiation of the authorisation procedure for clinical trials in more than one European member state by submitting a single application.
Developing new medicinal products is a long and complex process. After a pre-clinical phase of development and manufacture in conformity with GMP (“Good Manufacturing Practice”), new medicines must be evaluated in clinical trials, which asses the efficacy and safety of the product.
Every country within the European Economic Area, in which such a clinical trial is to be conducted, requires a national authorisation. While a separate procedure of validation, assessment, request for information, and approval/rejection was required for each country, the Voluntary Harmonisation Procedure has for several years been a tool for the initiation of an authorisation procedure across several countries selected by the applicant for conducting the clinical trial working together in the assessment.
The procedure was developed by the 'Clinical Trials Facilitation Group' (CTFG), a working group of the HMA ('Heads of Medicines Agencies'). For eight years, the Paul-Ehrlich-Institute (PEI) successfully coordinated this Network effort of national competent authorities.
The VHP reduced the period required for authorities to authorize a multinational trial to 60 days in all EU countries involved. Meanwhile, around 20 % of all applications for clinical trials to be conducted in more than one European country are submitted using the VHP.
Professor Klaus Cichutek, head of the HMA Management Group and president of the PEI said: “The HMA is proud that the Voluntary Harmonisation procedure has in the meantime been so well accepted by applicants world-wide, simplifying and reducing the period required for the authorisation of such multinational studies importantly, the VHP served as a model for the procedure to become applicable with the new regulation on clinical trial in future for the authorisation of multinational European clinical trials in Europe."
Compassionate use program
The EU regulatory framework makes it possible for non-authorized medicines to be made available under certain circumstances. This is achieved through a compassionate use program.
Relevant regulation
According to article 83 of Regulation (EC) No 726/2004, medicinal products without a Marketing Authorisation ‘may be made available for compassionate reasons to a group of patients with a chronically or seriously debilitating disease or whose disease is considered to be life-threatening, and who can not be treated satisfactorily by an authorized medicinal product.’
National jurisdiction
Compassionate use programs falls under national jurisdiction and, in most Member States under the remit of National Competent Authorities (NCA). Article 83 of Regulation (EC) No 726/2004, states that the Committee for Medicinal Products for Human Use (CHMP) has an advisory role at the request of a Member State. The individual NCA decide whether or not to approve the use of medicinal products without a market authorization.
The NCA in the Member State decides if such a program fulfils an unmet medical need according to their clinical practices and available alternatives. Some Member States have a long tradition on early access programs, including compassionate use, and others have different provisions in their national legislation.
Most of the compassionate use program notifications are submitted directly to the NCA within the different Member States.
NCAs that publish guidance on their compassionate use programs within their Member States | List | pdf
This list includes other early access schemes under article 5.
Colistin Resistance: The current human, food and animal situation
The use of colistin in animals and people in Europe varies greatly from country-to-country. It is used as an antibiotic of last resort in human medicine, with particular heavy use in cystic fibrosis patients in the community. Colistin is the antimicrobial with the 5th highest sales for use in lifestock in the EU[i]. The pattern of use in livestock amongst MSs is not indicative of uniform adoption of EMA’s Committee for Veterinary Medicinal Products (CVMP) best practice advice.
The European Commission requested in April 2013 a scientific advice from the EMA on the impact of the use of antibiotics in animals on public health and animal health and measures to manage the possible risk to humans. This was in accordance with the Commission "Action plan against the rising threats from AMR" adopted in November 2011.
The EMA advice of 2013 provided recommendations for colistin use in animals within the EU and indicated that they should be reviewed if there is a substantial increase of colistin resistance in animal bacteria and other new relevant information for public health.
To date resistance in bacteria to colistin had only been demonstrated in association with chromosomal mutations. A recent scientific publication[ii]indicated that in bacteria (Enterobacteriaceae) from pigs, retail raw meat (pork and chicken) and human patients in China a gene (mcr-1) has been found which enables horizontal (plasmid-mediated) transfer of resistance to colistin (polymyxins) between bacteria. This gene has now been found also in bacteria in Europe[iii],[iv],[v],[vi]. Since then, bacteria harbouring this transmissible colistin resistance have been reported from nearly all continents, and found also in ground beef, calves, chickens and turkeys. It has been found in archived material in the EU from as far back as 2005.
Based on this new evidence the European Commission requested in December 2015[vii] EMA to update its advice on colistin by 30.06.2016 at the latest. To undertake this work, EMA’s CVMP requested to reconvene the Antimicrobial Advice Ad Hoc Expert Group (AMEG), who prepared the 2013 advice.[viii]
[i] Fifth ESVAC report. Sales of veterinary antimicrobial agents in 26 EU/EEA countries in 2013. www.ema.europa.eu/docs/en_GB/document_library/Report/2015/10/WC500195687.pdf
[ii] Liu Y-Y, Wang Y, Walsh TR, et al. Emergence of plasmid-mediated Colistin resistance mechanism MCR-1 in animals and human beings in China: amicrobiological and molecular biological study. Lancet Infect Dis 2015 (Published online November 18, 2015: dx.doi.org/10.1016/S1473- 3099(15^00424-7').
[iv] Quesada, A. et al. Detection of plasmid mediated colistin resistance (MCR-1) in Escherichia coli and Salmonella enterica isolated from poultry and swine in Spain. Research in Veterinary science 2016; 105 pp 134-135
[v]Hasman, H. et al. Detection of mcr-1 encoding plasmid-mediated colistin-resistant Escherichia coli isolates from human bloodstream infection and imported chicken meat, Denmark 2015. Euro Surveill. 2015; 20(49)
[vi] Perrin-Guyomard, A. et al. Prevalence of mcr-1 in commensal Escherichia coli from French livestock, 2007 to 2014. Euro Surveill. 2016;21(6)
[vii] Request for an update of the 2013 advice on the impact on public health and animal health of the use of antibiotics in animals (colistin). Ref. Ares (2015) 5938235 – 18/12/2015. http://www.ema.europa.eu/docs/en_GB/document_library/Other/2016/01/WC500199646.pdf
[viii]Antimicrobial Advice ad hoc expert group (AMEG) Updating the advice on the use in animals of colistin - Mandate and rules of procedure. EMA/24480/2016
Multi Annual Work Plan adopted by HMA
After finalisation of the joint HMA/EMA strategy to 2020, the HMA developed a Multi Annual Work Plan (MAWP) to bring the joint overarching strategy into operation on the HMA level with the involvement of all National Competent Authorities. The MAWP has been developed by a HMA taskforce and was debated extensively in break-out sessions during the 2015 HMA plenary meetings in Luxemburg and Dubrovnik. The MAWP has been adopted on 17 February 2016 during the 83rd HMA meeting in Amsterdam.
Eleven topics were agreed as priority areas, namely:
- Antimicrobial resistance
- Availability of good quality appropriately authorised medicines
- Competence development programme through the EU Network Training Centre
- Developing an efficient, effective and collaborative approach on inspections to address sustainability
- Innovation and access to new medicines
- International collaboration
- Optimisation of the regulatory operations
- Responding to public and animal health emergencies
- Strengthen surveillance
- Implementation of the Telematics strategy
- Support for better use of medicine
Article 57 database – Variations – regulatory information
On 17 December the EMA MB considered that the Article 57 database is functional for the purpose of notifications of changes in QPPV and PSMFL information. From 1 February 2016 Marketing Authorisation Holders no-longer need to notify EMA (for centrally authorised products) and National Competent Authorities (for nationally authorised products) of changes to the QPPV or PSMF data by submitting a type IAIN variation.
Following the EMA MB decision the Commission has published the information on their webpage.
EU Medicines Agencies Network Strategy to 2020 adopted
The Network Strategy to 2020 by the HMA and EMA was adopted at EMA’s Management Board’s meeting on 17 December 2015.
- Adopted EU Medicines Agencies Network Strategy to 2020 | pdf
- Joint EMA/HMA press release | pdf
- Outcome of public consultation together with Annex 1 (Extract from minutes joint PCWP-HCPWP 4 June 2015) and Annex 2 (Summary of meeting with Industry Associations 23 June) | pdf
- Overview of comments – List of stakeholders | pdf
- Overview of comments – Written contributions | pdf
Workshop report on requirements for the authorisation of vaccines
The European Medicines Agency (EMA) has published the outcome of a joint HMA/EMA/industry workshop which explored how to ensure the availability of veterinary vaccines in the European Union.
How to improve the availability of veterinary vaccines in Europe
Transatlantic Trade and Investment Partnership (TTIP)
TTIP is a trade agreement to be negotiated between the European Union and the United States. The HMA Management Group send a letter to the European Commission with the request to give National Competent Authorities the possibility based on their expertise to provided their input on the chapter of PHARMACEUTICALS within TTIP.
HMA statement on the review of veterinary medicinal product legislation
The HMA provides a consensus statement on the review of the European veterinary medicinal product legislation.
Letter from Klaus Cichutek, Chairman of the HMA MG
Letter signed 10/04/15
HMA EMA common network strategy paper 2020
Making a difference to human and animal health
European Medicines Agency and Heads of Medicines Agencies consult on common network strategy to 2020 | pdf
The European Medicines Agency (EMA) and the Heads of Medicines Agencies (HMA) have released the ‘EU Medicines Agencies Network Strategy to 2020’, a draft common strategy to 2020 for the European medicines agencies network, for a three-month public consultation. Stakeholders are invited to send their comments before 30 June 2015.
The document under consultation outlines for the first time joint key priorities for the network and a high level strategy to achieve these.
The need to further strengthen the collaboration between the members of the network and work together towards achieving agreed goals has become more urgent recently. Europe faces the global threat represented by antimicrobial resistance to human and animal health, and needs to be prepared for emerging epidemics, as reminded by the outbreak of Ebola in West Africa in March 2014. At the same time the healthcare needs of patients in Europe are changing. Advancements in science and medicine mean that new and more complex medicines are being developed, which may bring opportunities for personalised medicines and more treatments for rare diseases. Patients also require timely access to new, beneficial and safe medicines. The globalisation of the pharmaceutical industry means that greater collaboration with regulators beyond the European Union is essential to assure the supply of safe, effective and good quality medicines for humans and animals.
The joint strategy for the European medicines agencies network is based on a coordinated approach and a strengthened collaboration within the network over the next five years, to address the challenges and make the most of the opportunities to benefit human and animal health.
The network is unique in the global regulatory environment. It includes all national medicines regulatory authorities for both human and veterinary medicines from Member States of the European Union (EU) and the European Economic Area (EEA), united in the Heads of Medicines Agencies (HMA), and the European Medicines Agency (EMA). By working closely together, the network can draw on the resources and expertise available across the EU, avoid duplication and share workloads.
The draft strategy focuses on areas where collaboration within the network can make a real difference to human and animal health in the European Union over the next five years. It builds on the EMA roadmap to 2015 and the HMA strategy document 2011-15.
The draft network strategy is arranged under four key themes focussing on:
· human health
· animal health and human health in relation to veterinary medicines
· optimising the operation of the network
· the global regulatory environment
Separate multi-annual work programmes/implementation plans for EMA, HMA, and coordination groups for mutual recognition and decentralised procedures, human and veterinary (CMDh and CMDv) will be developed in order to give detailed information on the work of each component of the network, and will also describe how the strategy will be taken forward.
All stakeholders are invited to send comments on the draft network strategic vision using this template to EUnetworkstrategy@ema.europa.eu no later than 30 June 2015.
Contact the HMA Permanent Secretariat
email: hma-ps@pei.de
03/25/14
Klaus Cichutek is the new chair of the HMA Management Group
On 19th March 2014, the HMA Management Group appointed from among its members a new chairman, Klaus Cichutek. The HMA MG consists of 5 permanent and two alternating members, the latter are heads of national competent agencies of the current and incoming EU presidencies (Greece and Italy). Klaus Cichutek is the head of the Paul Ehrlich Institute, the Federal Institute for Vaccines and Biomedicines in Germany.
07/03/13
Croatia - A new Member of the HMA
Croatia has finished accession negotiations and on 9 December 2011 signed the Treaty of Accession to become the 28th member of the EU. The ratification process was concluded on 21 June 2013 and entry into force and accession of Croatia took place on 1 July 2013.
Thus the HMA has a new member , the Head of the Croatian Agency for Medicinal Products and Medicinal Devices (HALMED), Viola Macolic Sarinic. Welcome!
01/04/13
21 December 2012: HMA raise concerns about discussion on progress on health claims on botanticals used in foods
The HMA express grave concerns regarding possible scenarios which are introduced in "Discussion paper on health claims on botanicals used in foods" published by the European Commission (EC). The outcome of this discussion may have a major impact on the future of the traditional herbal medicines regulatory regime, therefore every change of the current system should be evaluated very carefully to avoid any threats to public health safety. Read more
01/04/13
10 December 2012: HMA concerns regarding the adoption of the new Falsified Medicines Directive
The implementation of the Directive 2011/62/EU as regards the prevention of entry into the legal supply chain on falsified medicines is to strengthen existing quality control and health protection measures for medicines and to introduce new measures aimed at preventing falsified medicines and their components from entering the legal supply chain in the European Union. It should be noted that the Falsified Medicines Directive was not transferred into Directive 2001/82 for veterinary medicinal products. Read more